Nail fungus is a relatively dangerous phenomenon that can develop, destroying the entire nail plate. In the early stages of development, fungus can be invisible to the eyes, however, its negative effects on the structure of the nail plate are intensified daily. How to identify your own nail fungus and how to treat it, given the level of the disease, we will analyze further.

There are several signs that help determine the presence of fungal lesions on the nail plate:
- Nail loosen - you can check when cutting the nail edge. If in the process of nails, it is not cut, this is the first symptom of the presence of fungus and a clear opportunity to see a doctor.
- Nail plate thickening, especially on the edges of-hyperkeratosis (compaction) occurs due to the harmful effects of fungus that may interfere with the integrity of the nail fibers, which is why the last change in qualitative and quantitative form.
- The exception of its nails and cuts under the skin - such phenomena can trigger not only wearing tight shoes, but also fungal lesions that change the nail plate, providing the wrong location.
- Change of nail color (from pale to brown) - occurs due to the destruction of the active components of the nail plate and the folds of the protein cell during destruction.
- The presence of white plaque - fungal spores penetrates deep into the nail root, and also comes to the surface, which is dangerous for extensive infection of all toes.
The first signs that the nails have lost their health and have problems caused by the active activity of mushrooms, are:
- shine loss and surface gloss;
- a little bit of nails;
- Itchy wide itching from the entire leg, the appearance of red dot filled with transparent fluid;
- unpleasant foot odor, especially after a lot of sweating;
- Cross the skin on the heels and feet, wide rough.
These symptoms indicate a variety of problems with the feet, so it is best not to ignore the doctor's consultation. Early diagnosis greatly simplifies the treatment process, ensuring complete recovery.

Healthy feet in the feet: norms and deviations
To exclude or identify the presence of fungal diseases, you need to check your own feet, fingers and nails. The following clues should be maintained:
- Smooth feet, without corn, corn and seals.
- The skin is uniform, without cracks and spots.
- There is no redness and itching, especially between fingers.
- Flat nail plate, normal, transparent.
- Nail beds, surfaces with gloss look well.
In the event of a deviation from the standards stated, and the feet have an unpleasant spicy odor, a doctor's consultation and a review for the presence of pathogens are required.
Risk factors for fungal development in the foot
Fungal infections can occur anywhere, including home slippers. So this happens enough to have:
- weak immunity that cannot withstand active mushroom breeding;
- increased sweating, due to unelected and low quality shoes;
- presence of cutting in the nail area with unsuccessful nail cutting or cuticle;
- insufficient foot hygiene, as well as shoes;
- Frequent visits to public places where there is a high risk of infection: city baths, sauna, solarium, swimming pool, local beach;
- Excessive use of cosmetics (varnish, extension of nails, sprayers and refreshing gels), leading to the death of local immunity.
Separate types of mushrooms have different latent periods where the disease is not real.
You can be infected with fungus in two ways:
- Contact - through direct contact from sick people to healthy: personal hygiene items, public places, wearing other people's shoes.
- Contactly - Infection is due to the active development of the mushrooms in everyone's body. In certain situations (for example, a sharp decline in immunity), the number increases and cannot be completely controlled by the body.
Often, the following categories are subject to fungal lesions:
- Children with thinner layers of skin;
- people suffering from HIV infection;
- with increased sweating;
- The presence of chronic diseases that inhibit the immune system.

If there are any indications above, the condition of the nails on the feet and the overall stop is needed to be carefully monitored, paying proper attention to cleanliness.
Differentiation of fungal nail disease
In medicine, the concept of "fungal damage to the nails" is collective, as mushrooms of various types can act as pathogens. Often, such mushrooms are found on the toenails as:
- Dermatophytes - a group of mushrooms that manifest themselves in the form of a yellow spots or white vertical strips. The nails are infected gradually losing its strength and shape, after which the cavity becomes helpless and is easily removed from the nail bed.
- Yeast lesions - arising from the active activity of the genus Candida mushrooms. The nail itself is thinner, and the perioline roller squeezes and swells. It can be created as a free disease with frequent colds and poor immunity.
- Mold - located primarily on the surface of the nail, converts the color to the color of green, brown or white.
It is not possible to determine the agent of the fungal disease itself, as the same fungus, when exposed to a variety of aggregate factors, can appear differently. Therefore, it is impossible to start treatment, as each type of mushroom has its own antifungal drug that affects pathogenic life. Therefore, when diagnosing a slight deviation from the norm, you should consult your doctor, and take a test for the presence of fungus.
Level of fungal damage to the feet
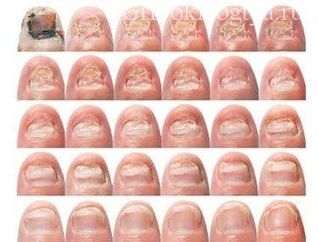
The process from the time of infection to the complete destruction of the nail plate is called the stage of the disease. Choose them 5:
- Infection - fungus enters the surface of the nail, plunging through the cuticle into the nail bed.
- Incubation period (from 3 days to 5 months) - mushroom activity is minimal, but it increases with lightning speed when all conditions are created for this: weak immunity, there is a wet warm medium, no proper hygiene. Outside, the incubation period is not created in any way.
- Early stage - the number of mushrooms is so large that it can negatively affect the viability of the nails. The edge of the nail plate gradually turns yellow from the edge to the nail bed. Nails get matte shade, healthy pink colors are gone, gloss disappears from the surface. In this case, the dry skin is observed.
- Active course level - the mushroom population reaches maximum, allowing you to infect other nail plates, after receiving a dispute through contact. Improved hyperkeratosis - increased production of keratin fiber, under the influence of fungal activity. In this case, the nails are compacted, apparently stand out on the surface of the finger.
- The final stage - determined by the killing of the nail plate due to the wound not only the nails, but also the nearby soft tissue. The entire surface of the nail has a yellow or brown shade, relaxation is recorded on the cut, accompanied by a painful sensation.
With large -scale infections, local symptoms can also participate:
- Dysbiosis in the form of stool disorders;
- increased body temperature;
- foot pain, increasing during movement;
- Confession Connection.
All of the above manifestations help determine the exclusive level of the onychomycosis course. To identify pathogens, you need to take a special analysis that shows the right genus and a type of fungus that causes onychomycosis.
How and what to treat
You need to understand that the key for successful treatment is the right diagnosis, which is impossible to do at home. Only doctors, based on analysis results, can identify the genus mushrooms, and choose the right treatment.
For many, it remains a mystery why, the antifungal drug purchased at the pharmacy does not help. There are many reasons and explanations for this. First, initially antifungal drugs are selected based on generators. Second, fungal treatment is a complex event consisting of:
- Local therapy - Apply antifungal drug to the nail surface.
- Oral antifungal tablets that can suppress fungal development and reduce their number from the inside.
- Medicines -immunostimulating medicines that "force" the body to produce a sufficient number of immune cars that fight the fungus freely.
- Compliance with foot hygiene is washed 2-3 times a day, with cold water and soap, after which they wipe dry with towels. The nails are cut every 3-5 days.
- Wear shoes made of pure leather, as well as cotton linen.
After being excluded at least one of these 5 points, the recovery process will be dragged for months, or even unsuccessful. Only comprehensive treatment will allow you to completely eliminate fungus, and do not include the risk of manifestations of relapse.
The recipe for traditional medicine, which is very difficult to cure nail fungus is in most cases ineffective. The result will appear only when the above suggestions to combat nail fungus lesions will be added.
Therefore, it is not difficult to determine the presence of fungus on the toenails. It is enough to do a nail plate inspection and all fingers in general, comparing it to a picture that shows the presence of fungus. Treatment is considered effective and correct only when it is carried out under the control of a specialist. Self -medication can have many negative effects on health, as well as complicate further treatment of the disease.
















